A new study published in the Journal of Neurological Sciences has highlighted the negative impact steroid-toxicities have on patient quality of life.[1] With an estimated 1% of the world’s adult population using oral glucocorticoids long-term, the costs are astronomical.[2]
Side effects that appear early on in treatment include insomnia, mood changes (anxiety, depression, anger issues) and hypertension. Long-term use can result in osteoporosis, bone fractures, cataracts and cardiovascular events.
The development of the Steritas Glucocorticoid Toxicity Index (GTI) in 2017 provided the first, validated clinical outcome measure of steroid-toxicity.[3] This clinician-reported instrument has since been used in clinical trials, clinical practice and large data set analyses in over 25 indications including severe asthma, systemic lupus erythematosus, polymyalgia rheumatica and myasthenia gravis.
The GTI, and related instruments that make up the STOX® Suite, look at steroid-toxicity from a clinicians’ perspective and may not necessarily capture the aspects of steroid-toxicity that are important to patients themselves.
Identifying the toxicities that have the biggest impact on patients
To address this, the authors of the recently published study set out to identify the steroid-toxicities that are most relevant to patients. Thirty-one patients with a history of glucocorticoid treatment and a diagnosis of myasthenia gravis, chronic inflammatory demyelinating polyradiculoneuropathy, systemic lupus erythematosus and vasculitis were recruited to the study. Patients were:
- Over 18 years of age
- Had at least one reported steroid-toxicity in the past year
- Received glucocorticoid treatment in the previous 6 months, with a minimum daily dose of 20mg
Study design was in accordance with recommendations for qualitative research on PROM instrument development by the FDA & ISPOR (Professional Society for Health Economic & Outcomes Research).
Data were collected using concept elicitation interviews (identifying information on symptoms and impact) that captured information on:
- Social and demographic parameters
- Medications: dosage (current & maximum)
- Experience of glucocorticoid toxicities and attributed side effects including:
- Severity, frequency and duration of toxicities
- Impact on daily life, social life and work/school productivity
- Disease history and disease-associated symptoms
Participants reported taking steroids for nearly a decade
The majority of the participants in the study were female and white, with a mean age of 51.8. More than half had a university degree or higher; consistent with the relatively narrow demographics that are typical of clinical study cohorts.[4]
The results highlighted both the magnitude of glucocorticoid use in these patients and the negative impact side effects had on their lives. Participants had been taking glucocorticoids for an average of 9.9 years and most (84%) were receiving glucocorticoids at the time of the study, with the majority taking prednisone. Those currently taking steroids had been taking them for an average of 7.8 months with an average daily dose of 15.2mg. Fifty-eight percent had received high-dose steroids intravenously at some point and the majority (87%), required additional medical tests such as bone mineral density testing to help monitor the impact of their steroid use.
Patients reported over 100 glucocorticoid-associated toxicities
Participants identified over 100 toxicities that they believed were associated with their glucocorticoid medications, with the most commonly reported toxicities being:
- Weight gain (87%)
- Increased appetite (84%)
- Insomnia/sleep problems (77%)
- Cognitive impairment/brain fog (71%)
- Easy bruising (68%)
- Anxiety (65%)
- Irritability/short temper (65%)
Individual toxicities were categorized into 13 domains (Figure 1) with toxicities in two of the domains - neuropsychiatric and metabolic - reported by all 31 participants. Almost all participants (94%) also reported at least one skin toxicity and over three quarters (77%) reported at least one bone toxicity.
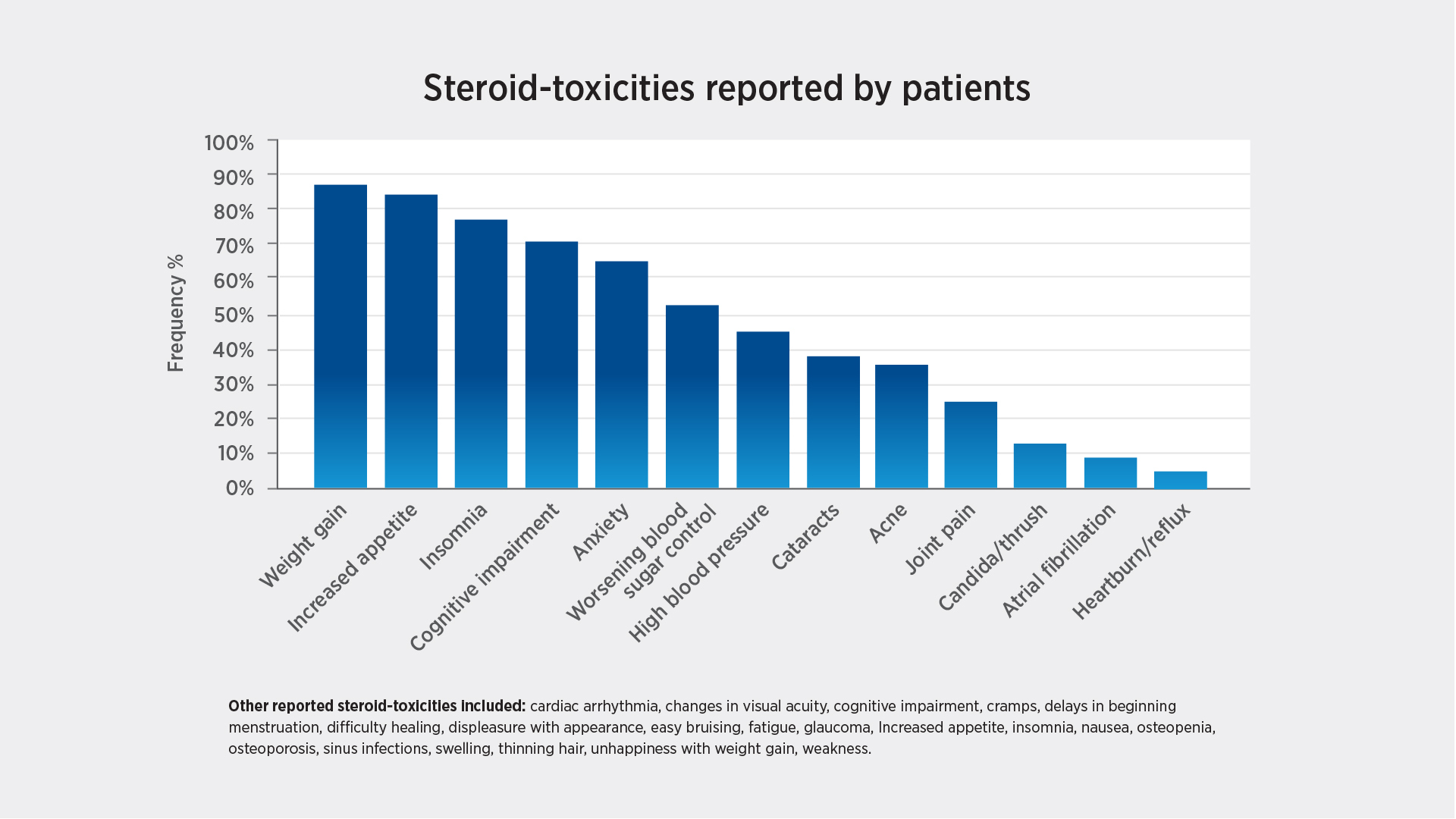
Figure 1: Most frequently reported steroid toxicities
What does this tell us?
The high frequency of toxicities reported by participants paints a stark picture of the impact that steroid-toxicity has on the lives of patients who are subjected to long-term steroid treatment. These “quantitative” data around the impact of steroid-toxicities are further illuminated in real-world context by the patients themselves. The comments collected are exemplified below, and provide insight into the impact of steroid-toxicity on the quality of life for the patients and their families.

Bone fracture
"I’ve had multiple rib fractures, I’ve had a sternum fracture, I fractured my tailbone, my ankle."

Irritability
“I went from zero to the Incredible Hulk in about 6 seconds, and I didn't even realize it was happening."

Easy bruising
“Absolute easy bruising. I just looked either like a drug addict or a domestic violence victim. It was bad.”

Muscle cramps
“It's usually when I'm asleep, and I already can't sleep, now I'm getting Charlie horses in my legs. Gosh, it's awful.”

Yeast infections
"Lots and lots of candida. Both in my mouth, tongue, and down my throat.”

Cataracts
“I had cataract surgery already. It probably was caused by prednisone because it was several years ago, so that's pretty young [for cataracts].”
This study not only highlights the importance of measuring and monitoring steroid-toxicity, but also that clinicians should work with their patients to minimize exposure to steroids with a plan to taper. It also underlines the importance of amplifying the patient’s voice on the toxicities they experience and their impact on quality of life.
The study and its results provide a perfect foundation for the next phase of development of the patient-reported outcome measure that assesses steroid-toxicity from the patient’s perspective.
References
- Howell TA, Matza LS, Stone JH, Gelinas D, Stone MN, Rao VTS, Phillips GA. Qualitative interviews to support development of a patient-reported companion measure to the glucocorticoid toxicity index. J Neurol Sci. 2024 Jan 30;458:122907. doi: 10.1016/j.jns.2024.122907.
- Fardet L, Peterson I, Nazareth I. Prevalence of long-term oral glucocorticoid prescriptions in the UK over the past 20 years. Rheumatol Oxf Engl 2011; 50:1982–1990. https://doi.org/10.1093/rheumatology/ker017
- Miloslavsky EM, Naden RP, Bijlsma JWJ et al. Development of the Glucocorticoid Toxicity Index (GTI) using multicriteria decision analysis. Ann. Rheum. Dis. (2017). 76:543-546. DOI: 10.1136/annrheumdis-2016-210002
- McCarthy A. Embracing Diversity: The imperative for inclusive clinical trials https://postgraduateeducation.hms.harvard.edu/trends-medicine/embracing-diversity-imperative-inclusive-clinical-trials#:~:text=Why%20Inclusivity%20Matters,accurately%20represent%20the%20broader%20population.
